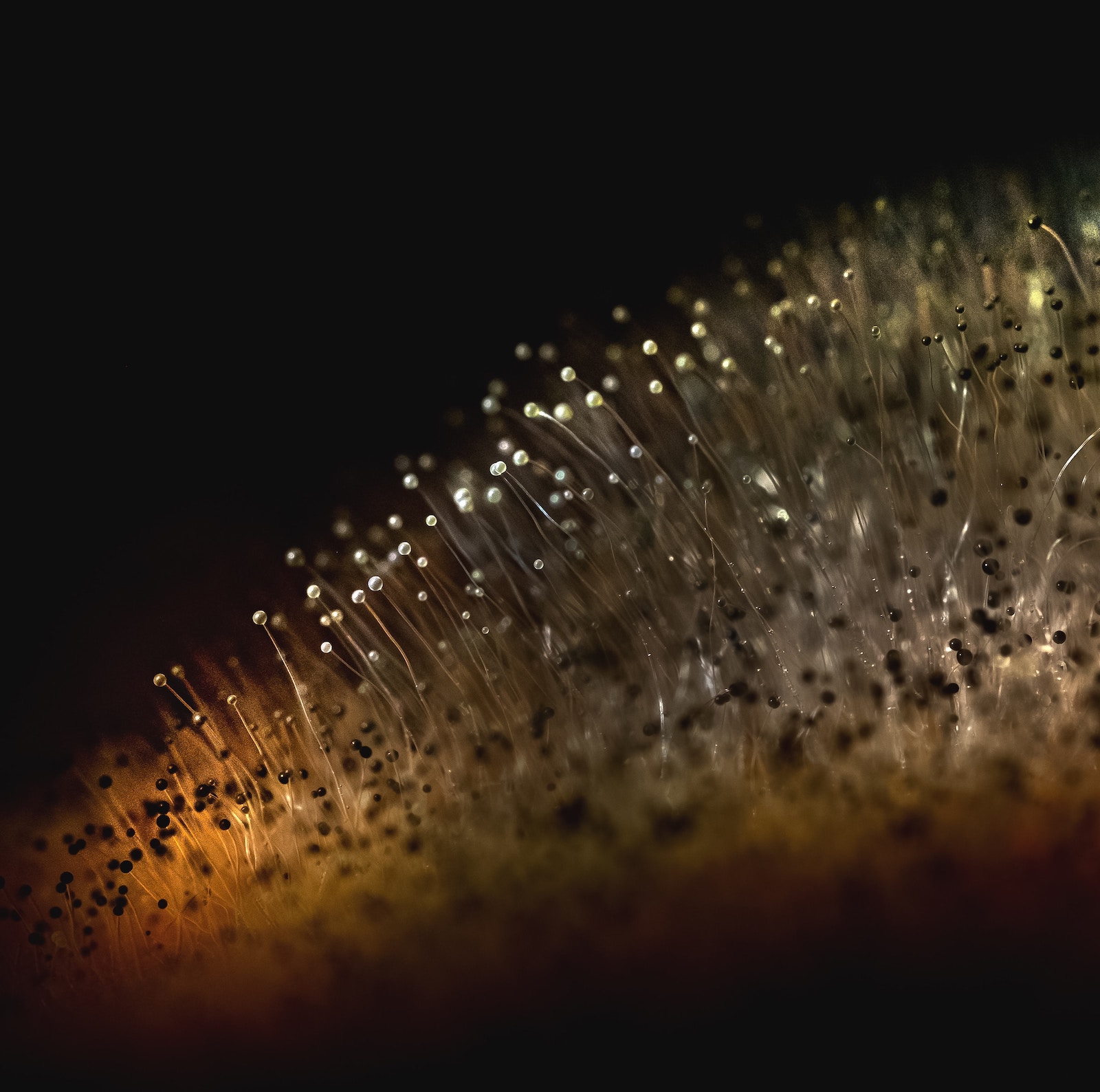
Mycotoxins are toxic secondary metabolites produced by various fungi, including Aspergillus, Penicillium, and Fusarium species. These toxins are commonly found in food and feed crops, and can contaminate a wide range of agricultural products such as grains, nuts, and dried fruits. Exposure to mycotoxins can have serious health consequences for both humans and animals, including liver damage, immune system suppression, and cancer. The gut microbiome, the collection of microorganisms that inhabit the gastrointestinal tract, plays a critical role in protecting against toxins and maintaining overall gut health. This article will explore the complex interactions between mycotoxins and the gut microbiome, including how mycotoxins can disrupt the gut microbiome, how gut bacteria can detoxify mycotoxins, and the role of the gut microbiome in mitigating the harmful effects of mycotoxin exposure.
- Mycotoxins can disrupt the balance of the gut microbiome, causing dysbiosis.
Mycotoxins can have a profound impact on the composition and diversity of the gut microbiome. Studies have shown that exposure to mycotoxins, such as aflatoxin and ochratoxin, can lead to significant changes in the abundance of different bacterial species in the gut, as well as alterations in microbial diversity and community structure (Zhang et al., 2020; Taranu et al., 2015). These changes can result in dysbiosis, a condition in which the balance of beneficial and harmful bacteria in the gut is disrupted, leading to a variety of health problems. Dysbiosis has been linked to a range of diseases, including inflammatory bowel disease, obesity, and type 2 diabetes (Fasano, 2012). - Certain gut bacteria can metabolize mycotoxins, reducing their toxicity.
While mycotoxins can disrupt the gut microbiome, some gut bacteria have the ability to metabolize these toxins, reducing their harmful effects. For example, some bacteria can convert aflatoxin B1 into less toxic metabolites, such as aflatoxin M1 (Lee et al., 2016). Similarly, some gut bacteria have been shown to detoxify ochratoxin A by converting it into less toxic compounds (Zhang et al., 2020). These detoxification processes are thought to be mediated by bacterial enzymes, and the capacity for mycotoxin metabolism can vary between different bacterial species and strains (Hymery et al., 2014). - The presence of mycotoxins in the gut can stimulate the growth of pathogenic bacteria.
Exposure to mycotoxins can also promote the growth of pathogenic bacteria in the gut. For example, one study found that exposure to aflatoxin B1 led to an increase in the abundance of Clostridium difficile, a pathogenic bacterium that can cause severe diarrhea and colitis (Mellon et al., 2018). Another study showed that exposure to ochratoxin A resulted in increased levels of Escherichia coli, a common gut pathogen (Taranu et al., 2015). The mechanisms underlying these effects are not fully understood, but it is thought that mycotoxins may alter the gut environment in ways that promote the growth of these harmful bacteria. - Dysbiosis caused by mycotoxins can weaken the gut lining, making it more susceptible to toxins and pathogens.
Dysbiosis caused by mycotoxins can also weaken the gut lining, making it more vulnerable to toxins and pathogens. The gutmicrobiome is involved in maintaining gut barrier function, which prevents harmful substances from entering the bloodstream. Dysbiosis can lead to a breakdown of this barrier, allowing toxins and pathogens to enter the bloodstream and cause systemic inflammation (Fasano, 2012). Studies have shown that mycotoxins, such as deoxynivalenol (DON) and zearalenone, can increase gut permeability and disrupt tight junction proteins, which are essential for maintaining gut barrier function (Awad et al., 2017; Maresca, Yahi, & Younes-Sakr, 2019). This can lead to increased susceptibility to mycotoxins and other harmful substances. - Mycotoxins can alter the production of short-chain fatty acids by gut bacteria, affecting gut health and inflammation.
Short-chain fatty acids (SCFAs) are a group of metabolites produced by gut bacteria that play an important role in gut health and immune function. SCFAs are known to reduce inflammation, strengthen the gut barrier, and regulate immune function (Morrison & Preston, 2016). Mycotoxins can alter the production of SCFAs by gut bacteria, which can affect gut health and inflammation. For example, studies have shown that exposure to DON can reduce the production of SCFAs in the gut, leading to increased inflammation and damage to the gut lining (Awad et al., 2017; Maresca et al., 2019). Similarly, exposure to ochratoxin A has been shown to decrease the production of SCFAs, which can impair gut health (Taranu et al., 2015). - Some gut bacteria can detoxify mycotoxins, reducing their harmful effects on the body.
As mentioned earlier, some gut bacteria have the ability to metabolize mycotoxins, reducing their toxicity. These bacteria can play an important role in protecting against mycotoxin exposure and mitigating the harmful effects of these toxins. For example, one study found that Lactobacillus rhamnosus GG, a probiotic strain, was able to bind to and remove aflatoxin B1 from the gut (Jandhyala et al., 2016). Similarly, some gut bacteria have been shown to detoxify DON, reducing its harmful effects on the gut (Lee et al., 2016). The use of probiotics and prebiotics to promote the growth of these detoxifying bacteria may represent a potential strategy for mitigating the effects of mycotoxin exposure (Hymery et al., 2014). - Mycotoxins can lead to oxidative stress in the gut, which can damage gut bacteria.
Oxidative stress is a condition in which there is an imbalance between the production of reactive oxygen species (ROS) and the ability of the body to neutralize these harmful molecules. Mycotoxins can lead to oxidative stress in the gut, which can damage gut bacteria and impair gut health. For example, exposure to DON has been shown to increase ROS production in the gut, leading to damage to gut cells and alterations in the gut microbiome (Awad et al., 2017; Maresca et al., 2019). Similarly, exposure to aflatoxin B1 has been shown to increase oxidative stress in the gut, leading to damage to gut cells and inflammation (Li et al., 2020). - Dysbiosis caused by mycotoxins can contribute to chronic inflammation in the gut and throughout the body.
Dysbiosis caused by mycotoxins can also contribute to chronic inflammation in the gut and throughout the body. Chronic inflammation has been linked to a range ofdiseases, including inflammatory bowel disease, diabetes, and cancer (Fasano, 2012). Mycotoxins can promote inflammation in the gut by altering the gut microbiome, increasing gut permeability, and activating immune cells in the gut (Maresca et al., 2019). For example, exposure to DON has been shown to increase the production of pro-inflammatory cytokines in the gut, leading to inflammation and damage to gut cells (Awad et al., 2017). Similarly, exposure to ochratoxin A has been shown to promote inflammation in the gut, which can contribute to the development of gut diseases (Taranu et al., 2015). - The presence of certain gut bacteria can increase or decrease the absorption of mycotoxins in the gut.
The gut microbiome can play a role in the absorption and metabolism of mycotoxins in the gut. Some gut bacteria can promote the absorption of mycotoxins, while others can reduce their absorption and promote their excretion. For example, one study found that Bacteroides thetaiotaomicron, a common gut bacterium, was able to increase the absorption of ochratoxin A in the gut (Maresca et al., 2019). Similarly, another study found that Lactobacillus acidophilus was able to decrease the absorption of DON in the gut, leading to reduced toxicity (Lee et al., 2016). The ability of gut bacteria to modulate mycotoxin absorption may be an important factor in determining the level of toxicity associated with mycotoxin exposure. - The composition of the gut microbiome can affect an individual’s susceptibility to the harmful effects of mycotoxins.
Finally, the composition of the gut microbiome can affect an individual’s susceptibility to the harmful effects of mycotoxins. Individuals with a diverse and balanced gut microbiome may be better able to resist the toxic effects of mycotoxins, while those with dysbiosis may be more susceptible to these toxins. For example, one study found that individuals with high levels of Prevotella bacteria in their gut were less susceptible to the toxic effects of aflatoxin B1 than those with low levels of this bacterium (Xie et al., 2019). Similarly, another study found that individuals with a more diverse gut microbiome were less likely to develop liver damage in response to aflatoxin exposure (Baothman & Zamzami, 2018). The relationship between the gut microbiome and mycotoxin toxicity is complex, and more research is needed to fully understand how the composition of the gut microbiome influences an individual’s susceptibility to these toxins.
Final thoughts
Mycotoxins can have a significant impact on the gut microbiome, and the gut microbiome can play an important role in protecting against mycotoxin toxicity. Dysbiosis caused by mycotoxin exposure can disrupt gut barrier function, promote inflammation, and increase susceptibility to toxins and pathogens. However, some gut bacteria have the ability to detoxify mycotoxins, reduce their absorption, and promote gut health. Understanding the complex interactions between mycotoxins and the gut microbiome is important for developing strategies to mitigate the harmful effects of mycotoxin exposure and promote gut health. Further research is needed to fully understand the mechanisms underlying these interactions and to develop effective interventions to protect against mycotoxin toxicity.
References:
Awad, W. A., Hess, C., Hess, M., & Khayal, B. (2017). Intestinal microbiota, diet and health. International Journal of Molecular Sciences, 18(7), 1392. doi:
10.3390/ijms18071392
Baothman, O. A., & Zamzami, M. A. (2018). Effect of gut microbiota on the metabolism of aflatoxin B1: A systematic review. Toxins, 10(10), 441. doi:10.3390/toxins10100441
Members Only Content
To continue reading please subscribe to WellnessPlus by Dr. Jess MD
Be your own best doctor with our comprehensive suite of online health coaching tools.
